By David Julian – The Natural Vitality Advocate
Why Amino Acids Matter on a Healing Journey
“Where do you get your protein?”
On the Medical Medium path, this question comes up a lot. But the truth is: it’s not protein we need—it’s the essential amino acids that build, repair, and heal.
In this post, I’ll share how I meet my amino acid needs without meat, dairy, or protein powders, and how I support deep healing of my brain, muscles, and nervous system.
What Are Essential Amino Acids (EAAs)?
Essential amino acids are the 8 amino acids (histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, valine) your body can’t make on its own. You must get them from food or supplementation to:
- Build and repair tissue
- Support neurotransmitters (serotonin, dopamine, GABA)
- Detoxify the liver
- Fuel your immune system
- Protect your nervous system
The Protein Myth (What Medical Medium Teaches)
“It’s not about how much protein you eat—it’s about how well your body can use the amino acids you give it.” – Anthony William
Medical Medium teaches that:
- Too much protein—especially from animal products—feeds viruses and overburdens the liver
- Protein powders are harsh on the kidneys and unnecessary
- Clean amino acids from fruits and greens are safe, effective, and healing
Where I Get My Amino Acids on the Medical Medium Path
1. Fruits
Fruit has been unfairly criticized in modern health trends, often blamed for everything from weight gain to blood sugar spikes. But the Medical Medium information sets the record straight—fruit is not the enemy. In fact, it’s one of the most life-giving, amino-acid-rich foods available to us.
Fruits are powerful because they offer:
• Bioavailable amino acids in a clean, non-inflammatory form
• Healing glucose that fuels the liver, brain, and every cell in the body
• Antioxidants and phytochemicals that neutralize toxins and oxidative stress
• Hydration through structured water naturally present in fruit flesh
• Natural antiviral properties that help reduce viral load and support the immune system
Some of my daily staples include:
• Bananas – rich in tryptophan to support serotonin and mood stability
• Wild blueberries – top-tier brain and nerve healers
• Mangoes, oranges, papayas – rich in vitamins, enzymes, and gentle detox power
• Apples, pears, figs and dates – grounding, soothing, and mineral-rich
I’ve made fruit a foundational part of my healing, and it’s helped me stabilize energy, lift brain fog, calm my nervous system, and support detox—without needing protein powders or processed snacks. Fruit is God-given, healing, and deeply intelligent in how it nourishes the human body.
2. Potatoes, Sweet Potatoes & Squash
Potatoes, sweet potatoes, and winter squash are often misunderstood, especially by those following low-carb or high-protein trends—but on the Medical Medium path, they’re absolute staples. These humble foods are clean, grounding carbohydrates that also happen to be excellent sources of amino acids in a highly digestible, healing form.
These healing root vegetables are:
• Rich in essential amino acids that support muscle repair, nerve function, and neurotransmitter production
• Packed with glucose, the preferred fuel source for the liver, brain, and immune system
• Supportive of adrenal health, helping stabilize energy and blood sugar
• Alkalizing and anti-inflammatory, aiding digestion and calming the gut
• Free from dietary triggers like fat, excess protein, and food chemicals that can burden the liver
I include them in my lunch or dinner almost daily—not just because they’re satisfying, but because they help rebuild tissue, support detoxification, and calm the central nervous system. They’re simple, healing foods that carry deep nutritional intelligence and align perfectly with how the body truly heals.
3. Leafy Greens & Herbs
I regularly include spinach, romaine, butter and leaf lettuces, cilantro, and parsley in my healing meals—either fresh in salads, juiced, blended in smoothies, or lightly steamed. These greens are far more than just roughage; they’re nutrient-dense powerhouses that provide some of the most healing forms of plant-based amino acids available.
These leafy greens and herbs are rich in:
• Bioavailable amino acids that help rebuild tissue and strengthen the nervous system
• Trace minerals like magnesium, calcium, and potassium that support adrenal and brain health
• Chlorophyll, which oxygenates the blood and helps cleanse the liver
• Electrolytes that stabilize cellular communication and hydration
• Natural antiviral and antibacterial compounds that help reduce viral load and inflammation
These aren’t just salad fillers—they are essential tools for regeneration, especially when healing from chronic illness, neurological stress, or immune dysfunction. I make it a point to include these greens in my daily routine to fuel detox, rebuild my nervous system, and support brain clarity.
4. Spirulina & Barley Grass Juice Powder (BGJP)
Included in my Heavy Metal Detox Smoothie, these superfoods:
- Rebuild tissues
- Support brain detox
- Bind and remove metals
- Fuel immune cells
5. Sprouts & Microgreens
I use a daily mix of organic alfalfa, radish, broccoli, and clover microgreens. This blend is rich in chlorophyll, trace minerals, and amino acids that are easily absorbed by the body and highly effective for cellular healing.
These microgreens are loaded with:
• Bioavailable amino acids to support muscle and nerve repair
• Enzymes that enhance digestion and detox
• Minerals that nourish the adrenals and brain
• Anti-inflammatory and antiviral properties that assist the immune system
I add a handful of this vibrant, living food to lunch or dinner each day as part of my commitment to rebuilding from the inside out. These tiny greens carry a tremendous amount of life force and healing energy—without burdening the liver or feeding pathogens.
Why I Personally Choose to Supplement with Essential Amino Acids
Even on a healing diet rich in fruits, greens, potatoes, and superfoods, I’ve found that sometimes the body needs extra support. This is especially true during periods of intense healing or physical rebuilding, such as:
• Brain and nerve recovery
• Post-seizure repair
• Detox from heavy metals or viral waste
• Muscle rebuilding and fitness recovery
• Chronic illness or long-standing deficiencies
For me, adding essential amino acid supplementation has been a way to fill in the gaps and help my body restore what’s been depleted over years of illness, neurological trauma, and detox work.
I want to be clear:
This is a personal decision that I’ve made based on my specific healing needs. It’s not something I believe everyone must do.
Some people may get all the amino acids they need from their diet alone—especially if their liver and digestion are strong, and they’re not dealing with the same level of neurological or muscular recovery that I am. Others may choose to use supplementation only temporarily, or not at all.
That’s the beauty of the Medical Medium path—it allows for flexibility and intuition.
We’re all walking different journeys, and I deeply respect everyone’s right to choose what feels right for their body.
For me, supplementing with clean, high-quality essential amino acids has provided:
• Greater physical resilience
• Faster recovery from exertion or flares
• Increased strength and stamina during detox
• Mental clarity and better emotional balance
• Support for neurotransmitters and nervous system repair
It’s not about pushing protein. It’s about giving my body the raw materials it needs—in a form it can absorb and use efficiently—so I can keep healing and living with strength, clarity, and peace. Supplemental EAAs help me fill in those gaps without stressing the liver. They’re fast-absorbing and highly effective for deep repair.
What Happens If You Don’t Get Enough Amino Acids?
While the modern world is hyper-focused on protein intake, it rarely discusses what really matters—essential amino acids (EAAs) in a form the body can actually use. Without them, the body begins to break down, struggle, and stall in its healing. This isn’t about protein deficiency in the conventional sense—it’s about a deficiency in the building blocks of life.
Even if someone is eating “clean,” they may still lack the essential amino acids needed for core functions like tissue regeneration, neurotransmitter creation, detox, and immune response. And on a healing journey, when the body is doing deep internal repair, those needs increase even more.
Here’s what can happen when the body doesn’t receive enough EAAs:
Muscle Breakdown
Without sufficient amino acids, the body will start to catabolize its own muscle tissue to access what it needs. This leads to:
• Weakness and loss of strength
• Soreness even after light activity
• Physical instability or poor posture
Especially when healing from chronic illness, injury, or prolonged detox, preserving muscle is critical—not just for mobility, but for supporting metabolism and nervous system balance.
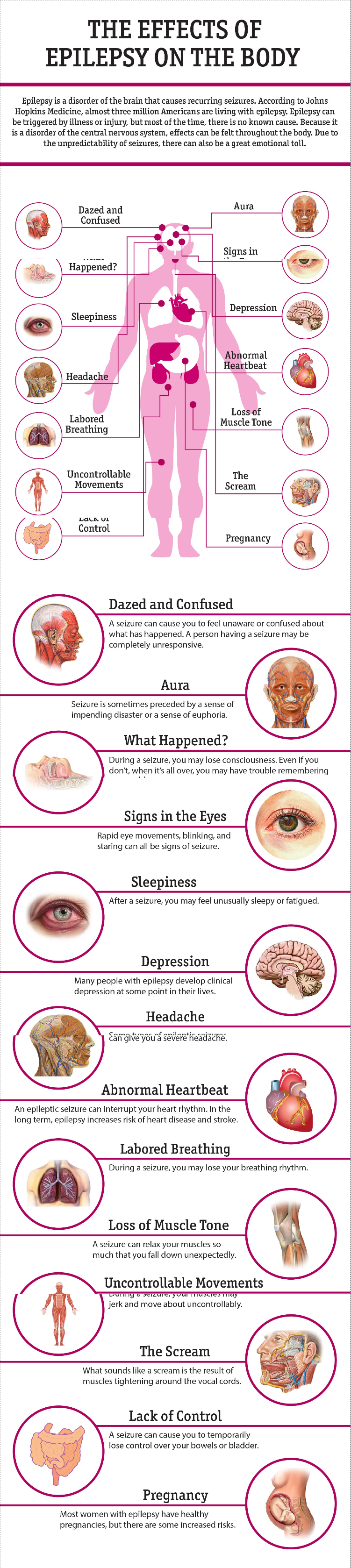
Neurotransmitter Imbalance
EAAs are the raw materials for brain chemicals like serotonin, dopamine, GABA, and melatonin. If the body doesn’t have enough:
• Brain fog becomes persistent
• Anxiety and depression can deepen
• Sleep becomes shallow or disrupted
As someone healing from neurological trauma, epilepsy, and PTSD, I know firsthand how crucial it is to keep neurotransmitters supported. Without adequate EAAs, emotional stability and mental clarity begin to slip.
Detox Stagnation
Your liver needs amino acids to build detox enzymes and carry out chemical conversions in both Phase I and Phase II detox pathways. Without them:
• The liver becomes overburdened
• Toxins recirculate instead of being eliminated
• Symptoms like skin breakouts, fatigue, and headaches flare up
In a Medical Medium lifestyle, we ask a lot of the liver—celery juice, HMDS, herbs, and more. But without amino acids, the liver lacks the fuel it needs to actually perform the detox.
Immune Weakness
Amino acids help create antibodies, immune cells, and repair damaged tissue from viral warfare. When deficient:
• Viral reactivations become more common
• Infections linger or recur
• Inflammation rises in the background
For anyone dealing with chronic EBV, shingles, or other hidden pathogens, EAAs are not optional—they’re required armor in the fight.
Poor Repair and Recovery
From skin to joints to hair, amino acids are needed for:
• Collagen production
• Connective tissue regeneration
• Hormonal balance and stress recovery
Without enough:
• Hair may thin or fall out
• Nails become brittle
• Wounds heal slowly or poorly
• Tissue pain or sensitivity can persist
Whether recovering from surgery, a seizure, or the wear and tear of daily detox, your body can only rebuild if it has the foundational materials—EAAs.
Bottom Line: You Can’t Heal Without the Building Blocks
We don’t have to overconsume protein to get these essential aminos—but we do need to get them from the right sources: fruit, greens, healing plants, and—when appropriate—clean supplemental support.
The difference between surviving and thriving often comes down to one question:
“Is my body being given what it actually needs to rebuild?”
When the answer is yes, healing deepens.
When it’s not, progress can plateau—no matter how perfect the rest of the protocol looks.
How Much Do You Need to Thrive?
Instead of counting grams, Medical Medium encourages focusing on absorption and clean sources.
Here’s my daily amino acid foundation:
- Fruits – Smoothies, snacks, and meals
- Potatoes/Sweet Potatoes – Lunch or dinner
- Leafy Greens & Herbs – Juices, salads, cooked dishes
- Spirulina + BGJP – Daily in my Heavy Metal Detox Smoothie
- Microgreens & Sprouts – Added to meals
- Essential Amino Acid Support – Used therapeutically as part of my healing plan
Clean Aminos Are the Key
I’ve learned firsthand that I don’t need animal protein to heal. What I need are the right building blocks—clean, plant-based amino acids that repair, protect, and fuel my recovery.
Thanks to Medical Medium’s teachings, I’ve experienced:
- Stronger energy
- Better sleep
- Faster muscle recovery
- Reduced seizure activity
- Clearer mood and focus
You can thrive on this path—without compromise.
Disclaimer:
The content on this site, including blog posts, shared material, and external links, is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional before making any changes to your health regimen, including medications, diet, exercise, or supplementation.
David Julian, Natural Vitality Advocate, is not a licensed medical professional. The views expressed in this blog and shared content are those of the respective authors and do not guarantee accuracy, completeness, or reliability.
David Julian is not affiliated with Natural Vitality or NaturalVitality.com. He does not promote, sell, or take a position for or against them.